Sacramento Observer
By Dr. Kermit Jones
October 6, 2021
OPINION – “You have weeks to live.” As a physician, I can assure you these are words we never want to utter after a cancer diagnosis. Sadly though, they are all too common. My philosophy is to treat patients like family, so when I encounter this devastating situation, I first and foremost feel deep compassion for the patient and their loved ones. That compassion quickly turns into frustration that, despite advancements and innovations in medical technology, we are still catching cancer too late.
It doesn’t have to be this way.
I will never forget the first cancer patient I ever treated. I was an intern at the Bethesda Naval Hospital in 2005, in my first month training as a doctor, when those words, “you have weeks to live,” shook me to my core for the first time. And it never gets easier. While I have had the great honor of treating many patients with cancer over the past 15 years, I have also experienced the horror that comes with their passing – the same gut-wrenching fate of my first patient, a life cut short, and a family left with incalculable loss.
If found early, most cancers have a 90% survival rate. On the other hand, late-stage cancer diagnoses generally have a 20% survival rate, which demonstrates that we need to do all we can to detect cancer early. Today, there are five cancers with Medicare-covered early detection tests: breast, colon, cervical, prostate, and some lung cancers. The availability of these tests has led to fewer deaths; however, 71% of the 600,000 cancer deaths each year are from types of cancer without a Medicare-covered screening. That’s 426,000 moms, dads, brothers, and sisters with lives cut short.
Fortunately, there is a bright light on the horizon thanks to the dedication of medical researchers to make cancer a disease of our past. Groundbreaking new detection technologies can detect up to 50 types of cancers through a simple blood draw, including pancreatic, esophageal, and liver cancers. Known as multi-cancer early detection screening (MCED), these tests hold the promise of extending and saving countless lives by finding and treating cancer before symptoms arise. MCED is perhaps one of the greatest opportunities we have to “end cancer as we know it,” like President Biden called for in February of this year. However, we won’t be able to realize the true benefits of MCED until it’s readily available to providers and patients alike.
Legislation now pending in Congress will help us reach that goal. Sponsored by Representative Raul Ruiz, MD, and co-sponsored by a broad, bipartisan group of representatives, the Medicare Multi-Cancer Early Detection Screening Coverage Act of 2021 (H.R. 1946) will create a new coverage pathway for MCED technologies approved by the U.S. Food and Drug Administration. Since 60% of cancers diagnosed are in people 65 or older, this legislation is a game changer. Its passage will not only transform how we detect the world’s deadliest disease but will ultimately help save more lives than ever before.
While this issue is important to me as a physician, it haunts me as a son. My 73-year-old mother, a nurse for more than 30 years, was diagnosed with Stage 4 lung cancer even though she had never smoked a day in her life. Because she wasn’t thought to be at risk for lung cancer, screening for the disease was not even on our radar. I can’t help but think about how much fear and pain our family could have been spared if her cancer had been found early through MCED. All of our loved ones should be afforded the opportunity to detect and fight cancer before it’s too late. I urge members of Congress and President Biden to join me in helping give cancer patients the chance at the life they deserve and pass H.R. 1946 without delay.
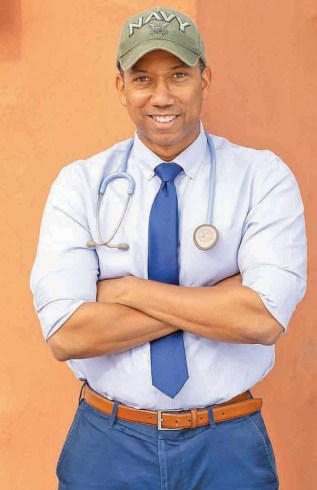
EDITOR’S NOTE: Dr. Kermit Jones is an internal medicine physician who serves patients in the Greater Sacramento area. He can be contacted via his website, kermitjonesmdjd.com